What exercises after a heart attack are best for me?
The best exercises to do after having a heart attack (myocardial infarction) are those that get your heart rate up and get you breathing slightly heavier. The aim is to get the blood circulating around your body so the muscles that need to move get a good oxygen supply.
As you have had a heart attack (or any other heart event) you need to be more careful when starting to exercise. You need to prepare your heart and the muscles for exercise so performing a gradual 15-minute warm-up is essential. Alongside the new medication you are taking it will help protect your heart from having to work too hard and shocking it into exercising.
At the end of any exercise session is it important that you do not stop and do a 10-minute cool down which helps prevent you from having a further event and also allows your body time to recover back to normal. Many people have a heart attack after exercise so it is important that you do not just stop what you are doing and sit down.
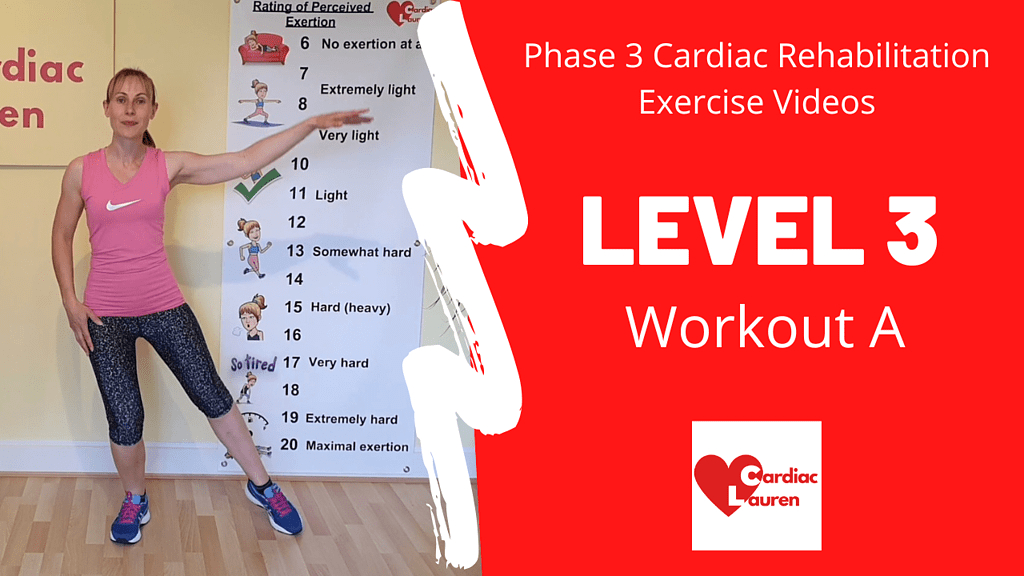
You will be invited to attend your local NHS Phase 3 Cardiac Rehabilitation programme if you have had a heart attack in the last few weeks.



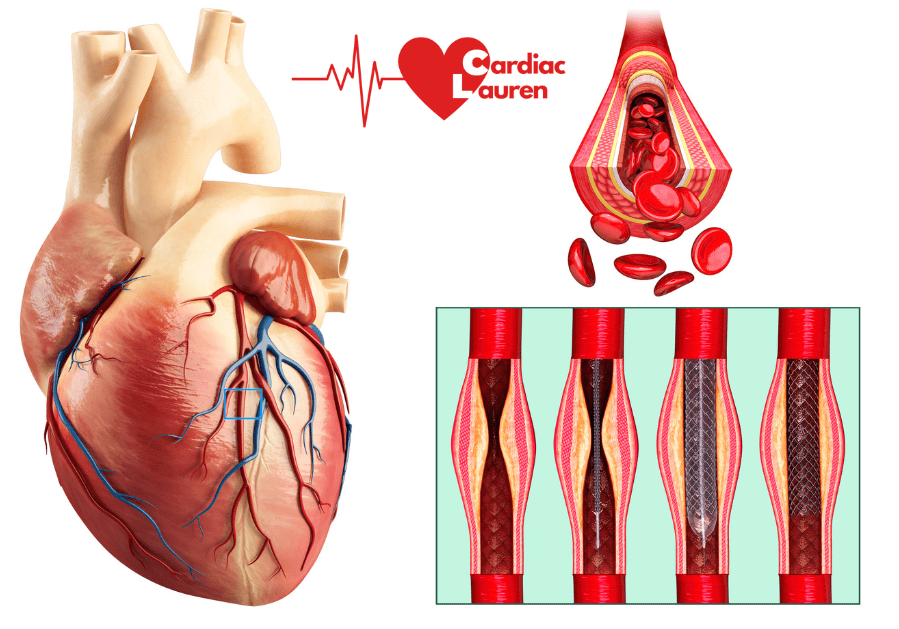
A heart attack can also be written as STEMI or NSTEMI on your hospital discharge notes. They stand for Non-ST-Elevation Myocardial Infarction and ST-Elevation Myocardial Infarction.
Leg exercises after a heart attack
Concentrate on leg movements as they are the best exercises to do after a heart attack. They will keep your overall blood pressure lower which in turn puts less strain on your heart. The natural response of the body to exercise means that by using these big muscles your arteries dilate and the muscles therefore get a good blood supply. This means they get a good supply of oxygen so they can contract and produce the action required to perform the exercise.
We use the leg muscles every day when walking, shopping, doing the housework and gardening, so it is important that we keep them strong and mobile.
Quadriceps (thighs)
Your thigh muscles are big and strong so these are the best muscles to work to help increase your fitness. When they are strong you can walk faster and longer, climb stairs more easily, get in and out of a chair without using your arms, and bending down and getting up will be easier.
Examples of thigh exercises (your quadriceps muscles):
- Squats/sit-to-stands
- Step/climbing stairs*
- Lunges
- Knee raises
- Marching on the spot



* Do not get out of your chair and go and climb the stairs numerous times without performing a warm-up. You will be putting your heart under excess stress and so are doing more harm than good *
Calf Muscles
Our calf muscles, the back of our lower legs, are key to improving our walking and balance. We use them all the time.
Examples of calf exercises (gastrocnemius & soleus muscles):
- Foot pedals (lift one heel off the floor at a time)
- Calf raises (lifting both heels off the floor)
- Walking – concentrate on pushing off your toes as you walk


Hamstrings
So our bodies remain balanced, you need to exercise your hamstrings which are the group of muscles in the back of your upper legs. Hamstring curls (kick your bottom) help get your heart rate up, they are good for increasing the range of movement of your knee and also they are important when balancing, walking and climbing.
Gluteals
Your buttocks, gluteal muscles, are strong muscles which you use when you are walking, standing, and balancing in everyday life, as well as during exercises such as squats, hamstring curls, stepping and many more. They help stabilise your pelvis and allow the movement of the leg in the hip in all directions.
Arm exercises after a heart attack
Concentrating on the lower body is best for a cardiovascular workout (getting your heart and lungs working), but we must not neglect our upper body. Arm exercises after a heart attack are just as important as many of us are weak around the shoulders, chest and upper back, our posture may not be great, so moving our arms is important. You do not even have to hold weights!
Examples of arm exercises:
- Biceps curls
- Chest press
- Shoulder press
- Lateral raises (sideways)
- Frontal raises (forwards)
- Wall press


* You MUST keep your feet moving when performing arm exercises * If not then your blood pressure can increase, blood will pool in your feet and ankles, and you are putting excess pressure on your heart to pump the blood back to your heart and you could pass out! *
In Cardiac Lauren we mix the exercises so you will do an arm exercise and then a leg one. At times you will put them both together, and on other occasions, you will be working on one side and then the other.
Abdominal exercises after a heart attack
These should only be performed at the end of a workout after the cool down. You can do all the main abdominal exercises ensuring that you do not hold your breath as you perform them, and do them in a slow and controlled manner as you will benefit from the exercise more than doing them quickly.
Try and avoid leaving your legs straight in the air as this puts a lot of pressure on your heart.
Example exercises after a heart attack
Watch example exercises after a heart attack that we do in Cardiac Lauren here.
Try Cardiac Lauren for exercises after a heart attack
If you are unsure whether signing up for a regular monthly subscription is for you, then why not try the 7 Class Challenge where you can try different themes over 14 days. This way you can find out which intensity level is right for you, get into an exercise routine at home, plus also work on your balance and strength alongside the normal exercises that get your heart rate up.