This video gives you a few tips on how to do a warm up and cool down when participating in various activities.
These activities range from housework, gardening & walking to cycling and swimming.
Transcript
Warm up and cool down for different exercises
Linking exercises to warm up, exercise component, and cooling down, and more like different activities.
Housework
So let’s think first of all about housework. Housework can be a form of exercise so your warm up is going to be going around the house tidying things up, putting things away, emptying the rubbish bins. Then your actual exercise is going to start building up from dusting and polishing,
actually into the cleaning. And you know you will definitely be exercising when you’re cleaning the bath, the kitchen, hoovering, mopping floors and you are going to get warm, hot and sweaty.
By the end of the session do make sure you just do a little mini cool stretches and leg stretches that we do in class. You are going to be reaching up and doing things and remembering to stretch out your triceps, your shoulders, your back, all of those stretches and the legs. So you really should do that after housework. But definitely if you’ve really put some good oomph into it, you can calculate that as part of your 150 minutes of exercise every week.
Gardening
Similar thing for gardening. So what you’re going to do, you’re going to go out into your garden, you’re going to walk around and work out ‘What do I need to do today?’ Just strolling around. If it’s in the summer, you might be doing some dead heading. You might be doing a bit of weeding. That sort of thing. Then you’re going to do maybe potting things up and your actual exercise, digging, mowing the lawn. In the autumn, you’ll probably find yourself brushing the patio, sweeping it, raking up leaves, lifting heavy pots, digging. Those of you with the allotments, it’s carrying water to water all your plants and then just turning over the soil and everything, preparing all of your beds for all your different fruit, vegetables and everything you’re growing on your allotment.
And again, after gardening for quite a lot of you, you’re going to be out there for hours. You’re going to be getting down onto your knees, you’re reaching, you’re leaning. You need to do a great deal of stretching when you do come in. Have regular breaks, stretch out all those leg muscles, the thighs, the backs of the legs, your buttocks, your back and all your upper arms. And then you will feel so much better the next day.
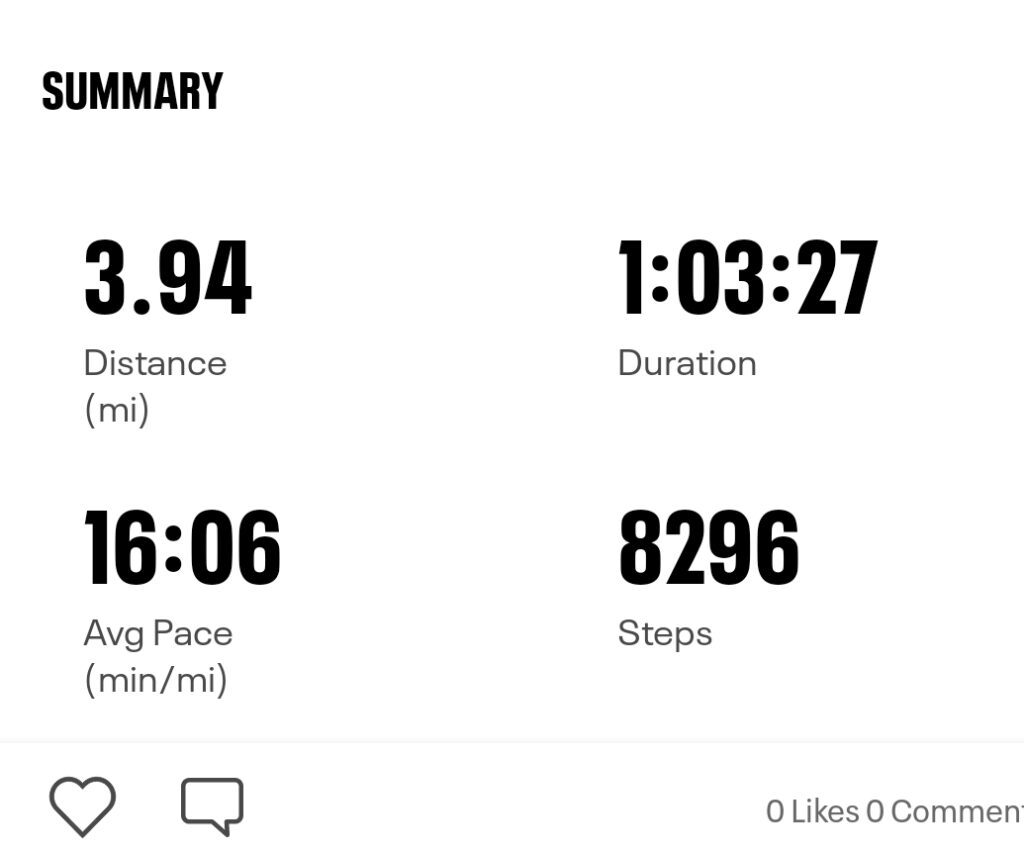
Walking – A to B, e.g. to the shops and back
Most of you will be going out for a walk, so if you’re walking, your warm up is just going to be, normally if you’re going from home to the shops, you’ve got to get your shoes on. In the winter, you’ve got to get your coat on. You’ve probably forgotten something and gone back upstairs or gone into the kitchen to get it. So rarely you’re ever going to go from your chair and then walk out the door. So you’ve probably done a bit of a warm up.
So just start walking a bit slower, gradually increase your pace and if you can get to a brisk pace because anything. Low to moderate pace is going to be classified as activity, whereas walking at a brisk pace involving heels is going to be classified as exercise.
So you’re going to start off slowly, gradually increase your pace as you get to your destination. Then you can start slowing down. So say you’ll go into the shops, you’ve gone out your house, you’ve done a good walk there. You slow down. You’re going to be walking around the shops. Ideally you’re going to be buying things. You’re going to be laden down with bags or rucksacks. On your way back you’re having to put a little bit more effort in.
Again, start a bit slower, increase your pace and then slow it down as you get towards your house. It’s one of those things again, you’re not going to literally walk in the door and stop and sit down. So you are going to do a bit of a cool down you’re going to put your bag down, you’re going to empty it, you’re going to take your coat off, take your shoes off, but if you have given it a little bit of oomph, do stretch out your legs and maybe you’ve been carrying anything heavy really mobilise all your shoulders and things like that. And so that’s how you just do a general walk from A to B.
Walking – a purposeful walk
Then if you want to go for a proper walk. So if you’re determined you’re going to go and drive somewhere. So Box Hill, those of you in Surrey, that is my example. You drive to the bottom of Box Hill, you’re not driving to the top, you’re driving to the bottom and you park at the bottom. Now one thing you must never do is just get out of your car and start walking up a hill. We don’t want to do that. Even if you live on a hill, you’ve got to try and walk down the hill first. Because that will just raise your heart rate and blood pressure too quickly.
So you need to then walk around the flat in the car park just to start with. Once you’ve done more of a warm up, you’re then going to start to walk up your hill. Now if it is a steep hill like Box Hill, then you’re just going to take it in little increments. There are great places you can stop and look at the vista. But do keep your feet moving. If you really need to sit down to catch your breath, just wiggle your toes and then continue when you can.
When you get to the top enjoy whatever it is, do slow down don’t just go huffing and puffing and then just go and lie down or something like that. Please just walk until you feel that you’ve calmed down, your heart rates calmed down, and then you’re not huffing and puffing.
When you do come down, if you’ve got dodgy knees, I know it sounds a bit strange, but zigzag a little bit and that just then doesn’t put too much pressure through your knee if you’re coming down straight. I don’t care what I look like, but you may feel that zigzagging is not quite for you. But you’re exercising still quite a lot by coming down a hill.
So once you get back to your car in the car park, don’t again just get in your car, drive off, please walk around on the flat again until you feel you’ve calmed down. And ideally, I would love you to do all the leg stretches, all of those that we gave you in class. So you’re going to stretch out your calf muscle. That’s the big stride forward. You bend the front knee, back leg is straight and heel is on the floor. You’re going to do the back of the leg. So you might perch yourself on the back on the edge of your chair, one leg straight in front of you, lean over nice and straight and feel a stretch from your bottom down the back of the leg. And then you’re going to hold on to something, you’re going to grab hold of your foot and you’re going to stretch out the front of your thigh for your quadricep stretch.
So if you really have gone for a purposeful walk, even if it is on the flat, please do your leg stretches afterwards.
Cycling
It’s a similar thing if you cycle again, you’re not just going to get out of your house and get on your bike instantly and go. You’ve got to go and get your bike. You’ve got to get the shoes on your helmet on, and again, just start off slowly, gradually increase your pace. Try not to do a hill too soon, but if your are on a hill, get yourself down into a lower gear. You want to feel like you’re exercising. You’re definitely going to get huffy and puffy, that is fine. But if it’s too much, stop. Get off your bike and walk. But if you do get to the top, it is normally either flat or downhill so you’ve got time to recover. So just be sensible with it. Please make sure you do stretch out your legs, especially your thighs after cycling. Again, don’t just stop when you get to your destination, walk around. Calm yourself down until you get back to your nice natural resting rhythm of heart. And breathing.
Racquet sports
Now if you’re going to do something like a racquet sport, you’re going to warm up as you would play in that racquet sport. So if you’re going to play badminton, tennis, so you’re not expected to do toe tapping and arms all out the place, you’re going to move directions, you’re going to move backwards and forwards. You’re going to just do knocking up. So you’re going to be using the body and it’s nice and easy just to get it all flowing, a good warm up again. And at the end of your session, stretch all those muscles. So again, you’ve been reaching with your arms, you’ve been twisting, your legs have been working. So your whole body needs a good stretch.
Football
It’s a similar thing if it’s like football, you’re going to mimic all your kicking, changing directions.
Pilates, Tai Chi, Yoga
If you do something like Pilates, Tai chi and Yoga, you would normally do a good warm up and cool down a stretch at the end.
Community classes, e.g. Zumba
Please do make sure that if you do decide to go and join an exercise class in the community, the warm up may be two minutes, 5 minutes, cool down two, five again if that. If it is a specific older adult class, you should then definitely get a longer warm up. But you know how important your warm up and cool down is, so do get to the venue early. Walk around, start doing your warm up before they do theirs, and then you know you’ve done a long enough warm up and it is safe for you. A similar thing for the cooldown, you just take that bit longer, you stay in the venue a little bit more, you walk around the studio or you just go outside, walk a bit more than do your stretches. So just be aware of that. The community classes may not do a long enough warm up and cool down.
Swimming
Now one other thing you may do is swimming. Now some of you will be allowed to go back and swim, some of you not. Most of you will have driven to the swimming pool if you have ridden your bike or walked and you haven’t had too much of a break in between getting there and getting changed into the pool and then you’ve done a bit more of your warm up. But otherwise most of you get in cold.
Do have that shower before you get in so then it’s not too much of a shock as you enter the swimming pool, you’re going to slowly get yourself in to the swimming pool into the shallow end and you’re just going to mobilise. So just stand in the shallow end. If you want to dip yourself under do. But do realise that does actually raise your heart rate and blood pressure without you knowing. So if you can do it just submerge to maybe waist that would be better. Mobilise your shoulders, mimic your breaststroke, mimic your front crawl. Kick your legs around, move your legs around. Do some walking on the spot, marching on the spot, then gradually submerge yourself. Stay close to the side and just start swimming really slowly.
Then as you gradually warm up, then you can start pushing yourself a bit more. But please be really careful in water.
When you are swimming and you’re thinking of your RPE scale, you may think, oh, this is RPE 11, this is really light, I’m going for a real easy swim. But actually your heart and your blood pressure have increased so much more because of the water pressure around your organs. So without you realising it, because you’ve got water all around your senses. All in your skin you don’t know you’re actually working harder than you are you don’t get the right responses so it’s very important if you think you’re working at RPE 11, you are actually working at RPE 13 so you’re working at that somewhat hard. So if you think you’re working at somewhat hard, so you’re a bit breathless you know your muscles are working you are actually working at RPE 14 to 15, which is that hard to hard heavy which is your cut off. So when you are in a swimming pool, please make sure you only work at RPE 13. Just be aware of that.
Once you finish your swimming session you’re going to come back to the shallow end. Ideally do stretches while you’re in the pool. So all the leg stretches, all the arm stretches, you could do it if you want to in the changing rooms but don’t wait till you get home because you will be a lot cooler by then. Wouldn’t say do it in the shower just in case you slipped and things like that. And just if you’re really not sure, always swim on the side of the pool so you can always grab the side if you need to stop at any time.
If you are interested in swimming, please make sure you do check with your cardiac rehab team if you are allowed to swim because certain heart conditions we do advise that you don’t swim.
I hope that all helps where you can just link different activities with your warm up, your cool down and remember to stretch as well.
Join us at Cardiac Lauren to learn how to do a safe warm up and cool down.